Efficiency-driven Anesthesia Modeling (EDAM)
The American Association of Nurse Anesthesiology recently developed Efficiency-driven Anesthesia Modeling, a new way of approaching anesthesia staffing.

Issues
- Physician anesthesiologist supervision adds unnecessary cost
- Medicare reimbursement is being eroded
Opportunity
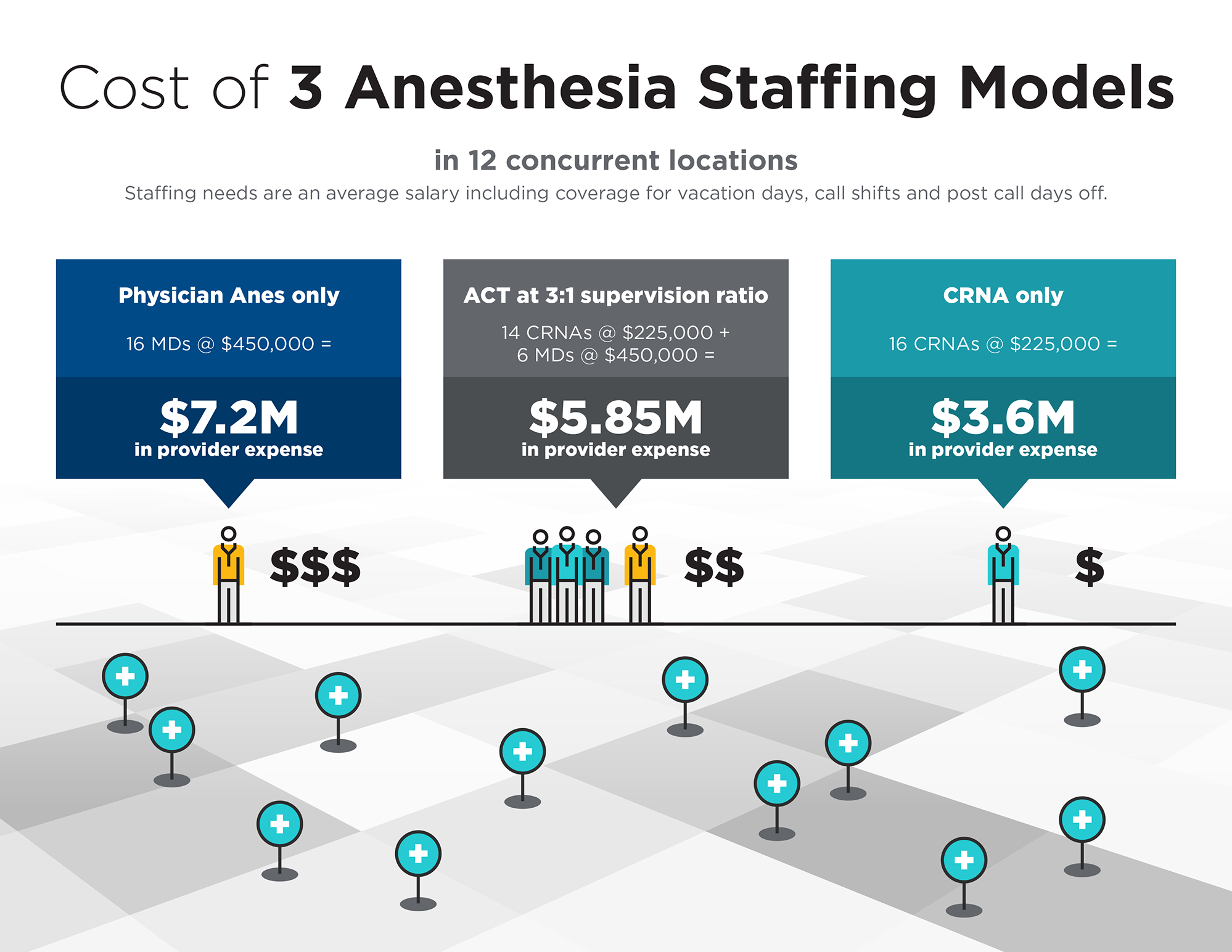
Landmark studies show the most cost-effective anesthesia delivery model is a CRNA working without physician anesthesiologist supervision.
A better way to preserve profits
In healthcare publications such as Becker’s ASC Review, experts maintain it is actually fiscally irresponsible to pay a non-revenue generating physician anesthesiologist two to three times the salary of a CRNA when the evidence has shown an additional provider does not improve quality, outcomes, morbidity or mortality.
Keep more of your Medicare revenue
Medicare pays the same fee for anesthesia services provided by a CRNA, a physician anesthesiologist, or both working together. CRNAs help protect Medicare revenue by providing lower-cost care than more expensive physician anesthesiologists.
Reduce surgical liability
CRNAs carry insurance coverage for all the services they provide. Excellent claims experience has brought CRNA malpractice liability premiums down an average 68 percent from 30 years ago, when adjusted for inflation. The downward trajectory continues.

Issues
- Patient safety cannot be compromised
- Outcome metrics are increasingly tied to reimbursement
Opportunity
There is no difference in safety and outcomes between CRNAs working alone vs. with a physician anesthesiologist.
In fact, experts predict an expansion of CRNA-only anesthesia services across the country in light of their near Six Sigma safety record and ability to provide high-quality, cost-effective anesthesia care.
CRNAs have a solid record of commitment to patient safety. Malpractice premiums for CRNAs decline every year even as their responsibilities increase, reflecting the value they bring to anesthesia care.
CRNAs spend more time with patients prior to, during and after surgical procedures, providing continuity, greater safety and an enhanced patient experience.
CRNAs have rigorous academic and clinical requirements for recertification, focused on clinical best practices and the latest advancements in patient care.
As care delivery becomes more accountable, the CRNA approach will continue to drive a higher standard of care and maximize outcomes-linked reimbursement models.

Issues
- Competition for anesthesia providers
- Lack of staffing flexibility
- Increased need for respiratory support care
Opportunity
As the need for anesthesia care grows, it becomes more difficult—and expensive—to recruit and retain physician anesthesiologists.
Perks physician anesthesiologists are asking for—and getting
Recent trends show a sharp increase in signing bonuses, among the highest amounts ever tracked. Paid relocation, paid continuing medical education, health insurance and malpractice insurance are standard offerings, as reported by physician search firm Merritt Hawkins. In addition, some search assignments include medical education loan repayments, which tend to be in the $80,000 range.
Physician availability is also impaired by burnout
A longitudinal study by Mayo Clinic shows a 43% higher likelihood that a physician would reduce their work hours in response to certain types of work pressures. Demographic changes also contribute; physician anesthesiologists are getting older, 55 years old on average.
Increasingly, CRNAs are filling the role
More CRNAs than ever before are mobile, working at several facilities. They maintain their own 1099 and locum tenens malpractice policies, increasing their ability to provide much-needed staffing flexibility.
The CRNA anesthesia staffing model provides facilities with the most cost-effective and versatile option.

Issues
- A serious need for personalized, non-opioid solutions
- Systemic lack of resources for chronic pain management
Opportunity
As with many social issues, overcoming opioid addiction requires boots on the ground.
Physician anesthesiologists often aren’t able to fully assess and manage post-surgical and chronic pain in the time they have with patients.
But CRNAs have that proximity, plus the knowledge, skills and commitment to move pain management forward, opioid-free. Collaborating with professional, governmental and community organizations, CRNAs across the country are actively leading in hundreds of initiatives to curb abuse and provide effective, responsible pain management.
These include:
Enhanced Recovery after Surgery (ERAS®)
Patient-centered, evidence-based, multidisciplinary team-developed pathways for a culture to reduce the patient’s surgical stress response, optimize physiologic function and facilitate recovery. These care pathways form an integrated continuum as the patient moves from home through the pre-hospital, pre-admission, pre-operative, intra-operative and post-operative phases of surgery and the return home.
Opioid Safety and Advocacy State Toolkit
AANA offers this toolkit checklist to provide guidance and help identify opportunities to create, lead or serve when asked to be involved in a state or community initiative.
Opioid Safety and Advocacy State Toolkit (PDF)
CRNAs Use a Multi-Modal Pain Management Approach which may Reduce Patient Need for and Reliance on Opioids
Many patients rely on CRNAs as their primary pain care specialist. CRNAs manage chronic pain in a compassionate, patient-centered, holistic manner, using a variety of therapeutic, physiological, pharmacological, and interventional modalities. The purpose behind this approach is to reduce the reliance on opioids as a primary pain management modality, thus aiding in the reduction of potential adverse drug events related to opioids, including addiction.





